When I was a graduate student at a School of Public Health in the late '70s there was, I believe, one remaining professor in the field of infectious disease, and he was on the verge of retirement. His expertise was in tuberculosis, but since TB had been conquered -- well, as had all infectious diseases, at least in the US -- the school was waiting for him to leave so they could put more resources into the truly important diseases of the late 20th century; cancers, heart disease, diabetes. These were caused environmentally rather than microbially.
This was still a few years before the first HIV/AIDS cases, and a while before resistance to antibiotics began to be widespread. So perhaps it was understandable that Public Health rather arrogantly lumbered toward the end of the century with infectious diseases relegated to the back burner.
This was more than just a change in the names on faculty doors. Infectious diseases have point causation: a single place and time of infection, and the one or few bugs that get in you and with high probability proliferate to produce disease. Environmental epidemiology was about multifactorial, statistical causation, by lifestyle exposures, of which each only acts probabilistically in proportion to the amount and duration of exposure. In a way, multivariate statisticians and computer analysis took the place of field epidemiology and laboratory research -- a pattern that Louis Pasteur had instigated in France in the 1800s, and so a profound change in expertise, outlook, and training of epidemiologists.
Then AIDS struck with a vengeance and brought TB along with it, broadsiding the medical and public health systems. Initially the gay community in the US was particularly hard hit, but after Public Health/safe sex measures got that under control, the epidemic became essentially contained within the poor, intravenous drug using community in the US, and ignored by the rest of us. So, still, infectious disease was not a problem.
Around about 1990, Ken contracted whooping cough, and so did our 8-year old daughter. This is a serious disease, killing millions before the vaccine was introduced. It's especially hard on infants. Not one of five doctors in town -- pediatricians, GPs and an ENT -- recognized it for what it was. One nurse told Ken that he couldn't have whooping cough because it had been eradicated. A GP told him that he might have whooping cough, but he couldn't diagnose it because he'd never seen it.
My father, a pediatrician, diagnosed Ken when hearing him coughing in the background during a phone call I had with him. He'd been vaccinated as a child, but immunity fades. Our daughter was susceptible because she only was given the first of the 3 recommended pertussis vaccinations as an infant after the one she did get made her sick, after which the doctor said whooping cough wasn't a risk and recommended she not have the rest of the series.
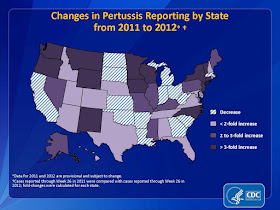
Ok, so pertussis hit our family decades ago, when whooping cough just wasn't on anyone's radar because, we thought, infectious diseases were under control. This year, though, pertussis epidemics have been declared in several states in the US, where they're seeing the highest number of cases in decades (e.g., Washington State). It's disconcerting to see that much of the information on pertussis on the CDC webpage about the disease was last updated in 2010, though there is this map of increasing incidence in the last year. Is this disease in fact on a whole lot more people's radar now than it was in 1990?
It was a BBC radio program that got me thinking about the disconnect between infectious disease reality and our perceptions. The July 31 "File on 4" was a discussion of the skyrocketing incidence of TB in the UK, and how poorly the system is prepared to prevent or detect this serious communicable disease. The program highlighted the cases of two young women with TB who were undiagnosed for far too long. One died still undiagnosed and the other lost a lung and now her quality of life because their GPs didn't even consider TB as a diagnosis.
Prevalence in the UK has risen dramatically, largely but not entirely in communities with recent immigrants from Sub-Saharan Africa and South Asia, where TB prevalence is high. Immigration services are not equipped to screen every traveler from high-risk areas for this disease, nor is the National Health Service. But a physician not even thinking to consider TB is as much an impediment to its control as the lack of screening services.
And, it seems that when screening is considered, it's for active disease via chest x-rays, but 100 cases in immigrants were caught on x-ray last year, while an estimated 10,000 latent cases went undetected, and it's latent cases that are the real threat. And, many of these are resistant to all known drugs used to treat the disease.
So, infectious diseases are again on the rise. Vaccine deniers are the subject of much concern, but they're just a small part of the problem. They essentially take advantage of the herd immunity provided them by the rest of us who do vaccinate our children, even if they may be responsible for small local outbreaks of various childhood diseases. The steady march of evolving bacteria, parasites, and viruses that we can only react to, not predict is a much bigger problem, as is the continuing spread of resistance to whatever antibiotics we care to throw at the bugs. The lingering expectation that we've still got infectious diseases under control -- indeed, HIV is now a controllable chronic disease -- is another impediment. Whooping cough has been eradicated, right? And of course the ease of global travel facilitates the spread of infectious diseases.
But there's another thing that we don't yet know enough about, and that is how much the chronic supposedly environmental diseases we've spent so many hundreds of millions of dollars trying to parse genetically actually are due to some infectious component. Genome-wide association studies (GWAS) have consistently found two things -- 1) multiple genes with very small effect and 2) many implicated genes associated with immune or inflammatory response. And this for a wide variety of diseases. So, it's possible that not only have we let classically infectious diseases creep back up on us with our eyes wide open, but that we've been treating other diseases as genetic when they are in fact infectious. One author in particular has been trying to refocus attention on infectious causes of 'environmental' disease: Paul Ewald at the University of Indiana. Others will be joining the chorus.
Infectious diseases are likely to have the last laugh.
Update: A discriminating reader writes to point out that Paul Ewald is at the University of Louisville, not Indiana.

Not to mention the connection between pathogens and so-called chronic diseases - they may not be classically infectious, but those rotten little scoundrels appear to be horning in there as well.
ReplyDelete